Improving MR operation to benefit staff, patient, and productivity
Imaging services are under constant pressure to respond to growing demand, shrinking budgets, system complexity, staff shortages, possible burnout, and COVID-19-related restrictions and requirements. In MRI, the technologists are at the center of operation; they are key to a successful high quality service and are critically valued by patients and referrers. Specific pain points experienced by MRI technologists emphasize the need for new approaches.
Read about daily operation experiences with existing and envisioned solutions to support technologists and benefit imaging departments.

Kris Giordano is Imaging Director at RWJ Barnabas Health. From 2011 to 2019 he was managing the MR section. He has been in the field of MR since 1995.
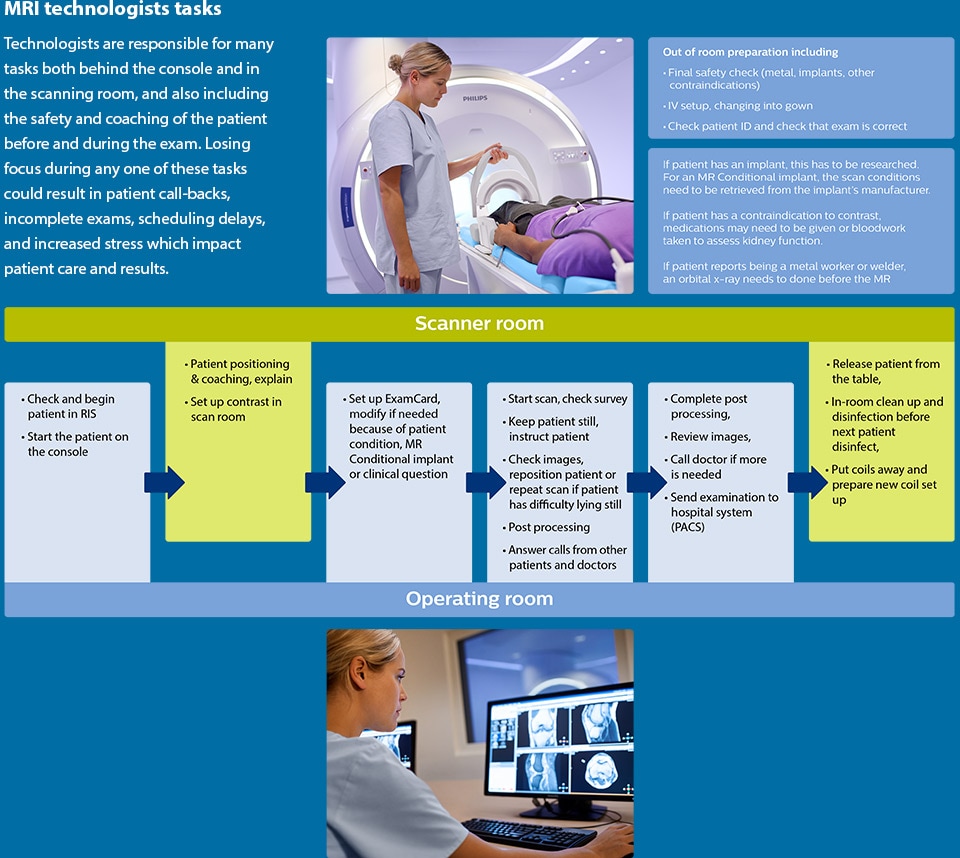
Technologists are at the center of MRI operation and have broad responsibilities
Technologists are in control of the MRI scanning process. Their duties seem ever-increasing and add to the pressure of always being up-to-date on the latest scanning techniques. Technologists must be well trained as well as knowledgeable about each patient's condition and the examination's purpose. They coach the patient and ensure patient safety. At the same time, they are expected to consistently produce high-quality images that allow radiologists to make a diagnosis.
Kris Giordano, Imaging Director at RWJ Barnabas Health in New Jersey, USA, says “About multitasking – I may not have enough time to truly describe the life of the modern-day MR technologist. So many tasks are now the responsibility of the MR technologists. In addition to scanning and the day-in, day-out necessity of meeting the demands of the patients, there are always telephone calls from patients, from radiologists, from colleagues regarding certain patient applications or prescriptions.”
“At the same time, everything that we do has to center on quality and safety. We have to ensure that we provide reproducible diagnostic quality, essentially contributing towards diagnostic confidence for the clinician. And we need to meet that demand without compromising safety in any way.”

COVID-19 has had substantial impact on role of technologists
In the past year, technologists’ broad responsibilities have evolved to not only include MR safety, but also additional COVID-19-associated measures. In the 2020 IMV report, 77% of respondents indicate that MR technologists have to wear personal protection equipment (PPE) such as masks, face shields, gowns, and gloves.1 The biggest change seen in MR operations was the cancellations and no-shows by MR outpatients due to fear of exposure to COVID and orders to remain at home.
“Since the COVID-19 outbreak, a main issue has been about reducing staff and patient anxiety”, says Mr. Giordano. “We no longer have 30-minute time slots, but have increased these to a standard of 45 minutes, and 60 minutes for the longer procedures, to allot the appropriate time for the proper cleaning of the equipment. Also, as we are triaging patients into Zone 3, we’re cleaning every room in front of them. We spray down the patient lockers and wipe the magnet in front of them. These tasks are costing us time, but are also instilling major confidence boosters in our patients.”
“Reduction of staff anxiety has been our number one focus. We ensured that we had adequate PPE and training on the donning of PPE for all levels of staff, including the concierge at the desk, radiology nurses, technologists, and radiologists. Creating a safe environment for staff has allowed us to ensure employee engagement sufficient enough to overcome the many challenges we are facing.”
“Since the COVID-19 outbreak, a main issue has been about reducing staff and patient anxiety”
Changing circumstances present new challenges
Imaging services operate with goals and boundaries in terms of financial outcome, number of procedures, quality and turnaround time of imaging and reporting, as well as patient satisfaction. Challenges can occur when declining reimbursements result in the need to scan more patients in order to break even. Further challenges may be associated with the COVID-19 pandemic, staff shortages, training and workload management, growing demand, long times between scan request and appointment, long times in waiting rooms for patients, and the need to be able to handle emergency cases in a timely manner.
“In general, we see that the demands for MRI are growing rapidly”, says Kris Giordano. “Even the orthopedics use seems to be broadening, which can create growing demand. Also, in our current mode of working past COVID-19, we’re tasked with an overabundance of patients, and I’ve been thinking a lot about what we can do to mitigate that burden.”
A growing population of patients with implants in particular require a substantial amount of attention from MR staff, who must first find out which implant the patient has, then find the MR scanning conditions from the implant manufacturer. Furthermore, setting up the scan to remain within these scanning conditions may require iterative adaptions of scan parameters. According to Mr. Giordano, “The collaborative team effort in researching MR implants really has been a major time crunch. This job alone, to complete that task prior to patient arrival, almost necessitates additional staffing.”
Growing demands provide opportunities for business expansion, but may also increase the pressure on imaging department and staff. When demand increases because new MRI capabilities have become available, additional training for technologists will need to be scheduled. Some sites have begun to try to reduce patient waiting times by increasing scanning throughput.2
“Working past COVID-19, we’re tasked with an overabundance of patients, and I’ve been thinking a lot about what we can do to mitigate that burden.”
Satisfaction of patients and staff goes hand in hand
“There is no patient satisfaction without staff satisfaction,” says Mr. Giordano. “So we must ensure that all levels of staff are happy and content in what they do. And especially now during this time of high anxiety and high pressure due to the pandemic, it is even more crucial than it ever was.”
Having a well-planned, well-managed patient schedule can benefit patients and technologists alike. It can allow the technologist to have more time to focus on the patient, which may in turn increase employee satisfaction.5
“Looking at options to improve both staff and patient satisfaction, we realized that one of our biggest issues are our wait times before start of the scan. We’re looking at ways to improve our management of patient delays and especially would like a more automated communicative measure to facilitate that better.”
“We must ensure that all levels of staff are happy and content in what they do,especially now during this time of high anxiety and high pressure due to thepandemic.”
Technologist overload affects department and patient
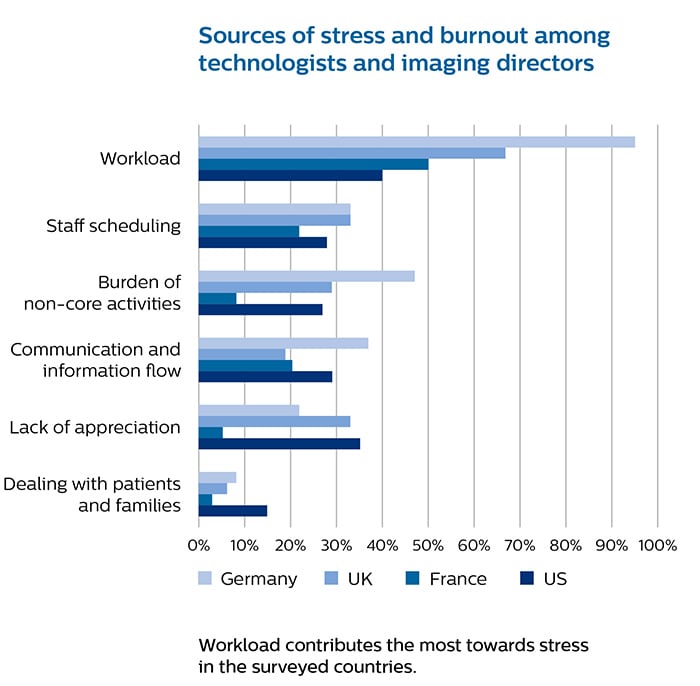
While technologists value their ability to provide excellent, patient-centered care, with a special focus on patient communication, their burden of responsibilities can detract from a technologist’s job satisfaction.3,4
In a 2019 study, substantial numbers of technologists reported moderate or severe levels of job stress, most often associated with their workload.3 Also inefficiencies, overtime, patients arriving late and no-shows, all contribute to job-related stress.
The study revealed that technologists are often asked to do more, for example patient transport, or to support imaging needs for other departments, leaving them less time for their patients.3 Technologists are sometimes unable to stay on schedule, and often experience having reduced time or no time at all for breaks.3
What are the consequences? Stress and increased workload may lead to mistakes and errors, which in turn may lead to retakes, recalls or complaints. Recent data has shown that high numbers of imaging studies and the complexities of the imaging care continuum still create several risks, including errors in scanning procedures, increasing undue stress for the imaging staff.3,4 Reduced satisfaction and stress can also lead to burnout. Prolonged stress may also take a toll on the technologist’s mental health, resulting in the possible development of anxiety and depression symptoms. 5,6
“This model of six per shift is great, but sometimes we are running into issues with staffing and coverage.”

Dynamics in the staffing model
In many countries, radiology department managers are facing growing demands in times where qualified technologists are hard to find. Determining the best staffing model can be an ongoing process.
“Having four scanners in our department, we usually have four technologists, one lead technologist or supervisor, and a radiology imaging nurse. This model of six per shift is great, but sometimes we are running into issues with staffing and coverage, so we rely pretty heavily on per diems in our modality”, says Kris Giordano. “I feel as though it’s inadequate, and we still need to have more people.”
Staffing is also influenced by the COVID-19 pandemic. “We’re looking at adding a technologist aide to help facilitate flow and help with the infection control mindset or even just helping out, for instance to help see a patient out or to help with navigating the building”, says Kris Giordano. “We have also seen a steep increase in cardiac MR, to the point where we’re looking at more facilitation, such as a post-processing software boost for our radiologists to expedite their read times. We’re really trying hard to meet the demands of today – yesterday is history for us, and we are assessing needs on a continual basis."
Improvements helping to ease the strain on staff
In the past years Philips has introduced a whole range of automation and other workflow improvements, such as automatic patient centering in the MRI, touchless respiratory triggering, in-room exam start button, automated planning and scanning, in-bore visual guidance for breath holds and scan progress, automatic adjustments for patients with MR Conditional implants, automated post-processing. And more will be coming.
Reliable automated processes and supportive tools present opportunity for gains in satisfaction and efficiency. The 2019 study shows that 23% of the imaging staff felt that almost a quarter of their work could be automated.3 It could allow technologists to multitask more easily, leading to higher throughput and resulting in more time for patients, which many of them desire.3 Increased levels of automation could also lead to robustness of quality, which helps further ease the strain on radiologists.7,8
Examples of automation in the operator room:
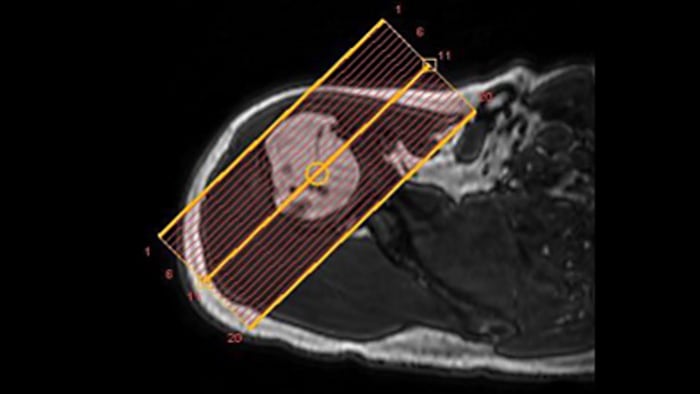
Automatic planning for consistent MRI results
“SmartExam gives me the confidence that I can present consistently planned images to the radiologist. At every interval of repeat imaging a patient’s images look nearly identical. This reproducible planning is crucially important in oncology patients pre- and post-treatment, in MS patients and more – everywhere the goal is the same: consistent imaging plan, consistent image plane, reproducible image quality,” says Mr. Giordano.
After learning the operator’s positioning preference, SmartExam can automatically and reproducibly position the scanning area

Automatic adjustments for confidence with MR Conditional implants
“The ScanWise software tremendously helps the technologist. It takes the guesswork and procedural adjustments out of the technologist’s hands and saves the time that the technologist would need for those adjustments. And on top of reducing time and number of clicks, it provides the confidence and peace of mind that we cannot exceed the limitations of the conditional implant – the scanner will keep parameters within bounds,” says Mr. Giordano.
In MRI of patients with MR Conditional implants the scanner can automatically adapt all sequences in the ExamCard to comply with the implant’s conditions after entering three parameters.
Automation can relieve need for training
Training and knowledge refreshers are essential for maintaining robust image quality and for ensuring patient safety. According to Kris Giordano, “Our technologists are fairly confident in the operation of the equipment. What helps is that our four MRI systems are all Philips, so they are similar in language and operation.” Having Compressed SENSE allows for reduction of actual scanning time in most exams, can leave more time for technologists to attend to their tasks and their patient.
Automated technology, including on-screen guidance for technologists, can reduce the amount of training needed, boost technologist confidence, and reduce stress levels. “We feel that automation tremendously helps us, and helps us focus on quality and safety,” says Kris Giordano.
Another observation is that technologists are multitasking on one monitor for scanning, post-processing and “filming”. Access to the daily patient schedule, as well as some post-processing often require different systems.
“We feel that automation tremendously helps us, and helps us focus on quality and safety.”

Towards a smarter user experience
Could a smarter user experience improve imaging workflow and create better experiences for technologists, patients, radiologists?
At Philips, we envision progressing towards more integrated workflows for patient scheduling, image scanning, post-processing and analysis to support facilities that aim to reduce patient waiting time, improve overall efficiency and reduce time to results.
Simplifying the user interface, more automation and harmonization between modalities may be the way forward for addressing many of the issues mentioned by users. Such improvements could make rotation of staff between different scanners or modalities easier and shorten training time, while reducing the need for refresher courses.
“When I think back to how Philips MRI system operations have improved over the past decades, I have no doubt that the next versions will also lead to better efficiency. Over the years, we have seen large efficiency gains in our modality, and it doesn’t seem to be slowing down in any way”, says Mr. Giordano.

Change starts with measuring
The task of making big changes is often coupled with big challenges. However, in many cases, using an incremental step-by-step process to make changes may be more feasible – with or without applying a strict continuous improvement methodology. Implementing several small changes simultaneously is often an easier process, and allows for the evaluation of the effect of each individual change.
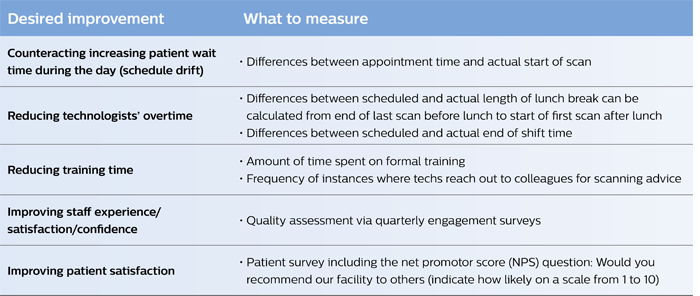
Measurements are needed, however, to ensure that the implemented changes lead to the desired improvement. This requires the determination of which measurable parameter will best reflect the desired benefit, and the proper timing of each measurement to ensure that enough data is collected to reflect both the “before” and “after” scenarios. The table below provides some ideas for useful parameters to measure in relation to the topics in this article.
To measure is to know. If you can not measure it, you can not improve it.
William Thomson, First Baron Kelvin,
British mathematical physicist and engineer (1824-1907)
References / potential sources
1. IMV 2020 MRI Market Outlook Report. December 2020. Accessed 23 January 2021. 4. Research report: The patient factor: Imaging Beyond the Scan. 2017. www.usa.philips.com/c-dam/b2bhc/master/Specialties/opportunity/staff/documents/the-patient-factor-final.download.pdf 5. Zhu J, et al. Prevalence and influencing factors of anxiety and depression symptoms in the first-line medical staff fighting against COVID-19 in Gansu. Front Psychiatry. 2020;11:386. 6. Wu W, et al. Psychological stress of medical staffs during outbreak of COVID-9 and adjustment strategy. J Med Virol. 2020;92:1962-1970. 7. White Paper: Realizing productivity gains in MRI. Focusing more on the patient can boost the efficiency of MRI procedures. 2018. www.usa.philips.com/healthcare/consulting/articles/white-paper/mri-efficiency-white-paper 8. Nandwana SB, Walls G, Reich S. Learning From Experience: Minimizing Patient Delays in Radiology: Optimizing On-Time Starts for CT Procedures. Curr Prob Diagn Radiol. 2021;50(1):11-15. 9. Scanning patients with MR Conditional implants. Philips FieldStrength 2015. www.philips.com.au/healthcare/education-resources/publications/fieldstrength/mri-and-mr-conditional-implants 10. Staff shortages in imaging departments causes stress among existing employees. Radiology Business 2018. www.radiologybusiness.com/topics/healthcare-economics/staff-shortages-causing-stress-among-employees Results from case studies are not predictive of results in other cases. Results in other case may vary.
2. Hospitals and Health Systems Face Unprecedented Financial Pressures Due to COVID-19. American Hospital Association. www.aha.org/guidesreports/2020-05-05-hospitals-and-health-systems-face-unprecedented-financial-pressures-due. Accessed 22 January 2021.
3. Research report: Radiology staff in focus. An impact and satisfaction survey of radiology technologists and imaging directors. 2019. www.usa.philips.com/healthcare/medical-specialties/radiology/improving-radiology-staff-and-patient-experience/staff-research Accessed 20 January 2021.
